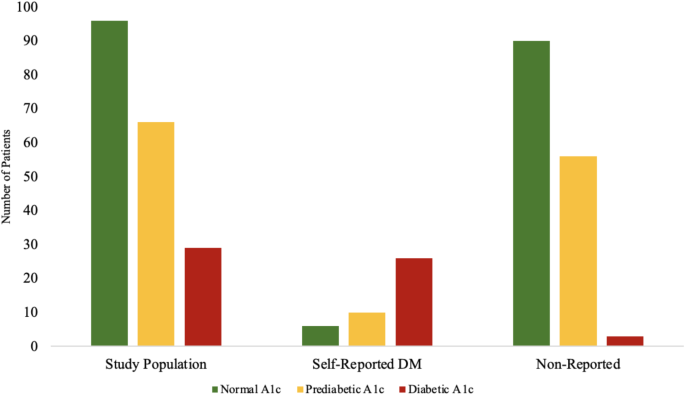
Results from this study demonstrate a high prevalence of diabetes and prediabetes in a food-insecure population in West Chicago. Within the study population, 50% of patients had an abnormal A1c (A1c ≥ 5.7%), 35% of which had a prediabetic A1c and 15% had a diabetic A1c. Chronic hyperglycemia is associated with cardiovascular disease, peripheral artery disease, and additional micro and macrovascular disease13,14. Furthermore, diabetic patients are two to three times more likely to experience myocardial infarction or stroke, with additional morbidities including chronic kidney disease, stroke, and neuropathy14,15. The observed high prevalence of prediabetes and diabetes in food-insecure individuals is concerning due to the potential morbidity and mortality of sustained hyperglycemia. This demonstrates the necessity of implementing targeted interventions to mitigate the progression to T2DM in prediabetic patients.
Over 22% of screened patients self-reported T2DM, almost double the national prevalence of 10.7%16. This suggests that there is an increased prevalence of diabetic patients in food-insecure populations, a finding consistent with previous literature11. Food insecurity is a public health issue and is associated with worse health outcomes including hypertension, diabetes, coronary heart disease, congestive heart failure, stroke, chronic kidney disease and obesity12,17. Lack of access to healthy, cost-effective food options results in overall poorer diets and is associated with poor glycemic control, low diabetes self-efficacy, poorer self-management behaviors, more depressive symptoms, lower medication adherence and lower blood glucose monitoring18,19. Often due to budget constraints, food insecure individuals are relegated to purchasing lower-quality, non-diverse food contributing to weight gain and increased susceptibility to developing diabetes and limiting disease management18,19.
Among those who did not report a history of T2DM, 38% had a prediabetic A1c and three patients had a diabetic A1c. Prediabetes is associated with an increased risk of mortality and cardiovascular event rates, and if unmanaged, increases one’s likelihood of developing diabetes5,20. In a 30-year follow up study, Gong et al. reported that among the pre-diabetics in the control group, 95.6% progressed to diabetes reported progression to diabetes21. Due to the significant chronic comorbidities associated with diabetes and disease progression, accessibility to healthcare is crucial for disease diagnosis, monitoring, and mitigation. This is of particular concern for food insecure populations who may face barriers precluding consistent access to healthcare resulting in worse glycemic regulation.
Of those who self-reported DM, 43% presented with A1c greater than 7%, indicating uncontrolled T2DM. This finding, along with overall elevated levels of diabetes and prediabetes, indicate a struggle amongst food insecure individuals to control their sugar levels. While many factors may contribute to elevated rates of uncontrolled diabetes the inaccessibility of consistent and routine healthcare creates a significant burden22,23. Barriers related to insurance status, economic stability, reliable transportation, and other social determinants of health increase the difficulty of accessing healthcare, delaying diagnosis, preventing longitudinal monitoring, and rendering pharmacologic therapies unattainable22,23. Our data underscores the importance of community-based, preventative screening as a means to identify at-risk patients and provide strategies to mitigate the risk of developing T2DM and associated complications.
Obesity is a significant risk factor for diabetes and prediabetes with national data estimating that more than 80% of pre-diabetics are overweight or obese24. The participants in this study had an average BMI of 31.06 in the self-reported group compared to 28.66 in the non-reported group (p = 0.096), both values corresponding with overweight categories. Lifestyle modifications and robust health education can help combat many barriers affecting food insecure patients. Dietary modifications and exercise interventions that promote weight loss, confer a significant improvement in glycemic control5,25. Gong et al. reported that the lifestyle modifications group had a lower incidence of diabetes, 26% lower incidence of cardiovascular disease events, 35% lower incidence of microvascular disease and all-cause deaths were 26% lower21. In patients already facing barriers to care—financial, transportation, or otherwise—lifestyle modifications are effective measures to reduce the burden of disease in disadvantaged populations. Improved health literacy, such as education on simple and complex carbohydrates, how to interpret food labels, and realistic exercise techniques, empower patients to make personalized changes directed at improving glycemic control.
Community based health initiatives such as CHI target the root causes of health disparities. Through meeting patients in a non-hospital setting in their community centers, patients are offered comprehensive cardiometabolic screening and education irrespective of insurance, transportation, or financial status. Through motivational interviewing techniques, patients receive robust education on their glycemic status. Individualized health counseling highlights the importance of exercise, nutrition and other accessible lifestyle modifications to improve individuals’ cardiometabolic profiles. At screening events, nutrition experts incorporate affordable recipes, cardiologists and medical students provide health coaching targeted at improving health literacy, and social workers connect patients with primary care physicians and healthy food options. In order to mitigate the health disparities that exist in the United States, further research must be done to understand how social determinants of health (SDOH) such as food insecurity play a role in chronic conditions such as DM.
Limitations
Due to a limited sample size and self-reported histories of DM, the generalizability of the presented findings are limited. More screening efforts are needed to illuminate the prevalence of prediabetes and diabetes in a food insecure population.